Fluorescence Microscopes
Automated Fluorescence Microscope Transforms Process for Induced Cancer Stem Cell Research

Dr. Hideyuki Saya
Professor of the School of Medicine, Keio University
M.D. Ph.D., Division of Gene Regulation, Institute for Advanced Medical Research
Dr. Hideyuki Saya was born in 1956. He completed a doctorate program at the Graduate School of Medicine, Kobe University in 1987. After receiving a Ph.D. in medicine, he studied as a Postdoctoral Fellow at the UCSF Brain Tumor Center in 1987. He was then appointed Assistant Professor at the University of Texas MD Anderson Cancer Center in 1988. From 1994 to 2006 he was Professor of the Medical Oncology Course at the School of Medicine, Kumamoto University before taking his current position as Professor at the Institute for Advanced Medical Research, Keio University School of Medicine in 2007. Dr. Saya specializes in tumor biology. He has received many awards, including the Hoshino Memorial Lecture Award (2000), the Victoria Jursnich Carhart Memorial Lecture Award (2000), and the Deborah M. Richman Memorial Lectureship (2001).
Get detailed information on our products by downloading our catalog.
View Catalog
Understanding the mechanism of cancer development and metastasis using artificial cancer stem cells and aiming to establish a useful foundation for drug discovery
Dr. Hideyuki Saya is studying front-line cancer treatment based on the theme of molecular mechanisms of cancer development and malignant transformation at the Division of Gene Regulation, Institute for Advanced Medical Research, Keio University School of Medicine. As the first professor of the Institute, Dr. Saya aims to contribute to the prevention, diagnosis, and treatment of cancer and other refractory diseases by applying the knowledge and techniques cultivated through advanced basic research to clinical medicine. His efforts are focused on the basic research for the treatment of brain tumors and other cancerous lesions using biological approaches centering on molecular targeting.
We’re here to provide you with more details.
Reach out today!
01. Understanding the mechanism of cancer by focusing on cancer stem cells
Cancer is a disease that develops when the mechanisms connected to growth arrest, cell death, and aging suffer a problem as a result of the genes becoming unstable due to mutations in tumor suppressor genes and activation of oncogenes in cells with propagation ability.
It was conventionally believed that a cancer tissue is a clump of cells that proliferate endlessly, but it has been revealed in recent research that there are two types of cancer cells. One type is called cancer stem cells. These cells possess a self-renewal function and can keep making progeny cells almost permanently. The other type makes up the majority of cancer cells and eventually loses the ability to propagate. In other words, it was found that cancer cells also have a relationship similar to normal stem cells and progenitor cells.
One characteristic of cancer stem cells that makes cancer difficult to treat is their slow cell cycle, which reduces the susceptibility of these cells to anticancer drugs and radiation. This means that even when most of the cancer cells die off from chemotherapy, the cancer stem cells still survive. This leads to the problem of the inability to reach a complete cure for cancer.
Dr. Hideyuki Saya, professor of the Keio University School of Medicine, studies the cell cycle control mechanism and cell adhesion control mechanism using a cell biological approach for detailed analysis and verifies the results using animal models. His research is aimed at understanding the mechanisms of cancer development, invasion, and metastasis on a molecular level.
We’re here to provide you with more details.
Reach out today!
02. Exploring therapies based on the concept of molecular targeting
After graduating from the School of Medicine at Kobe University, Dr. Saya sought to become a neurosurgical clinician who treats brain tumors. However, he was faced with the reality that 95% of the patients with malignant brain tumors die within 2 years. Due to the limitations of today’s chemotherapy and surgical treatment, he decided to go into research at a graduate school to find a treatment himself. Nevertheless, he came to realize that there is a huge barrier to overcoming brain tumors, as he puts it: “While I earned a Ph.D. at graduate school, I found almost nothing regarding treatment.”
In 1987, upon completing his doctorate program, Dr. Saya started his studies at the Brain Tumor Center of the University of California San Francisco. As the UCSF Brain Tumor Center was researching the world’s most advanced cancer treatment, he thought he could learn about the newest and most up-to-date techniques and treatments. At UCSF, Dr. Saya worked on the genetic analysis of brain tumors and focused his efforts on exploring target molecules that can lead to treatment. At the time, the concept of “molecular targets” was still a progressive approach and gave Dr. Saya critical inspiration that led to his later work.
The following year, Dr. Saya was appointed Assistant Professor at the Neuro-Oncology Department of the University of Texas MD Anderson Cancer Center. As this facility was the largest cancer treatment institute in the United States, Dr. Saya was involved in cancer research on a wide range of cancer sites, including brain tumors.
In 1994, Dr. Saya was invited to be the first professor upon the establishment of a basic research course on tumors called the Medical Oncology Course at the School of Medicine, Kumamoto University.
At Kumamoto University, he embarked on research into the cell cycles of different cancers, including brain tumors. The cell cycle is a process in which daughter cells born from cell division grow into mother cells, which further divide into new daughter cells. Dr. Saya focused on the possibility that understanding the mechanism of the cancer cell cycle can provide insight into stopping the proliferation of cancer cells. Therefore, he quickly introduced a method that enables time-lapse observation of cell division and thoroughly conducted basic research. His reason for this approach was because he had seen numerous cases where “drug discovery research would almost invariably collapse if you were only looking at applied research without doing any basic research” during his studies in the U.S.
We’re here to provide you with more details.
Reach out today!
03. Cell-based drug screening
While Dr. Saya has achieved great results in drug discovery research targeting the cell division mechanism mentioned earlier, he is also well-known for his research on the CD44 cell adhesion molecule. CD44 is a molecule that adheres cells to each other, and according to Dr. Saya’s research, it is believed to be the key molecule in tumor metastasis. By controlling this molecule, we may be able to block cancer invasion and metastasis.
Based on this two-pronged approach that is at the forefront of the world’s cancer research, Dr. Saya is aiming to develop a molecular target drug that is effective against brain tumors and other refractory cancers. While research in this field is progressing gradually around the world, no research institute has yet established a system for testing the efficacy of drugs under conditions close to a living body. Dr. Saya says, “In vitro* experiments based on cultured tumor lines have showed that there are effects. However, it is our greatest research challenge to investigate what is actually going on in the human body. If we can get over this wall, we will have taken a giant step towards screening for drug discovery.”
However, research using bio-mimetic models is not easy. Simply put, while the environment of a cell culture plate is two-dimensional, a living body is three-dimensional. On top of that, the latter has various intermingling structures, providing cancer cells with many places to hide. The efficacy of a drug varies by site. How to overcome this problem of heterogeneity is the big question. In other words, a key point of research is how to reproduce an environment close to a living body through the use of an in vitro method that uses cells.
Conventionally, it was common to perform screening with just the enzyme in the test tube when creating an inhibitor for an enzyme. In contrast, Dr. Saya’s lab is testing the efficacy of drugs on a cell basis. In this approach, cells are cultured under special conditions to reproduce a pathological condition that occurs in a living body. These cells are then used to observe changes caused by compounds. In recent years, the way drug discovery is pursued has been changing drastically, as exemplified by Dr. Saya’s efforts. Dr. Saya points out that drug screening is currently shifting from enzyme-based to cell-based techniques.
* in vitro: an experimental environment in a test tube. The contrasting concept is “in vivo,” which means an environment within a living organism.
We’re here to provide you with more details.
Reach out today!
04. Successful production of induced cancer stem cells (iCSC)
The latest research Dr. Saya has been working on is cell differentiation control anomaly analysis and cancer drug discovery research using induced cancer stem cells, adopted as a Core Research for Evolutional Science and Technology (CREST) by the Japan Science and Technology Agency. By applying the iPS cell production technique, Dr. Saya genetically engineered normal mouse cells and successfully induced them into becoming cancer stem cells (iCSC: induced cancer stem cell) that have self-renewal, differentiation, and tumorigenic abilities.
Dr. Saya plans to explore the mechanism of tumor formation using different iCSCs while aiming to screen compounds and antibodies that can control tumorigenesis. Currently, his research uses mice, but it aims to eventually produce iCSCs from human normal type cells to use as targets for the development of cancer treatment drugs.
In the latest research based on cancer stem cell theory, the use of drugs that target the progeny cancer cells and cancer stem cells separately is being considered. It is a therapeutic approach that first kills the progeny with treatment drugs and then targets the cancer stem cells—which therapeutic drugs did not previously work on—with another drug. This approach is believed to have the chance to dramatically improve therapeutic benefits.
We’re here to provide you with more details.
Reach out today!
05. Fluorescence microscope without the need for a darkroom drastically changed research
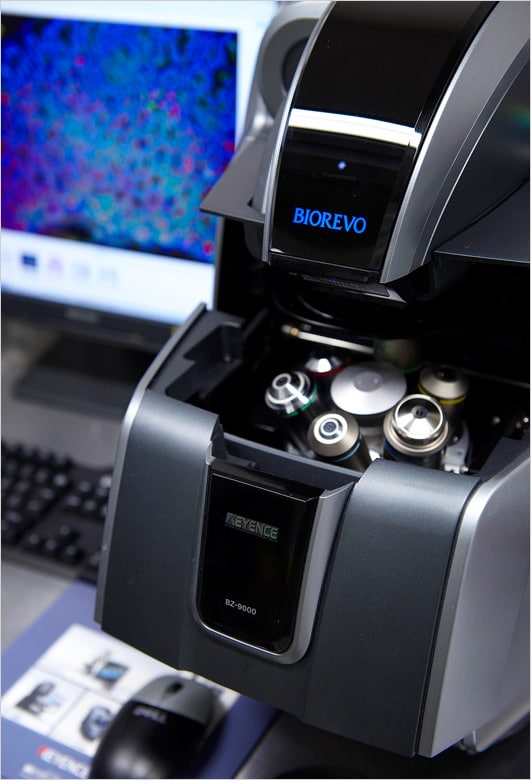
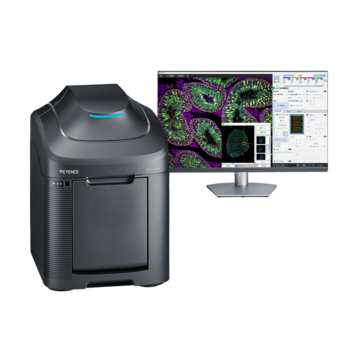
The BZ Series installed in the Saya Laboratory. The compact design of the BZ Series means that it does not take up very much space.
With current trends leaning toward an increasing focus on cell-based research for cancer treatment, Dr. Saya mentions that image observation is being given more weight and the role of microscopes is becoming increasingly important. He says, “Three-dimensional observation is crucial for thoroughly examining the changes in cancer cells. Also, counting the cancer cells in addition to observing them is necessary for verifying heterogeneity. Microscopes that support quick observation as well as measurement are in demand.”
From his extensive experience with cell-based research reaching back to his school days, Dr. Saya says that fluorescence microscopes have been and are essential instruments. He reflects back on the difficulties in the old days: “Every day I would lock myself up in a darkroom for more than 3 hours for observation.I used to shine a pocket light at my hands when I was sketching pictures of cells. However, this task was inefficient, not to mention it was straining on my eyes.”
For this reason, he was surprised when he saw KEYENCE’s BZ Series fluorescence microscope for the first time at a demonstration during his term at Kumamoto University. “Being able to observe on the monitor instead of through an eyepiece was epoch-making. We decided to install the BZ Series because we got many requests from students wanting to use it.”
We saw results soon after the installation of the BZ Series.Dr. Saya reflects on observations becoming easier due to the usability of the BZ Series in brightfield microscopy. “Another great advantage was that I could give explanations on key points and instructions on experiments while looking at the monitor with a group of students. This was unthinkable when using microscopes equipped just with eyepieces.”
While compounds are generally singled out for screening in current drug discovery, efficient screening is still essential as the number of candidates can be in the thousands to tens of thousands. It is fair to say that the ability to capture images and observe rapidly depends on the quality of the microscope.
Dr. Saya, who believes that the sharing of information is important in educational settings, also mentions that he deliberately leaves the cell images clearly displayed on the monitor screen. According to Dr. Saya, by ensuring that such images are seen by students in the lab, students become more interested and realize how important it is to take clear images, thereby becoming motivated to do so. Dr. Saya says, “Sharing research findings through images results in the level of the entire lab improving.”
We’re here to provide you with more details.
Reach out today!
06. BZ Series contributes to research efficiency
Specimen of continuous sections of an organ. All the images were captured in about 1 hour.
One of the big criteria for Dr. Saya when selecting a research instrument is whether it helps make research faster.At the same time, he also respects how many researchers in the lab can or want to use it. Dr. Saya says, “In that sense, almost everyone in the lab uses the BZ Series. I also regard it highly in terms of its reliable operation—with no mechanical failures—despite its high utilization rate.”
For cell-based observation of cancer invasion and metastasis using a mouse, continuous sections of an organ need to be examined. Twenty to thirty strip preparations are necessary for each organ, and he says that this is a number that cannot be processed in a short time with conventional ocular microscopes. However, by using the BZ Series, all image captures can be completed in approximately 1 hour.
Dr. Saya also has high regard for the image stitching function, which rapidly and seamlessly joins images after wide-area imaging. “When I publish images at an academic conference, I often get questions from attending researchers about how I took them,” says Dr. Saya.
A three-dimensional observation in a bio-mimetic environment is required for detailed examination of cancer cell proliferation, and he mentions that the XY-Z-axis stage is useful in vertical-axis observation.
Dr. Saya also adds that he often uses the cell count function to measure how many cancer cells are contained in a given density. This function is becoming increasing important in this age where observation needs to be quantified.
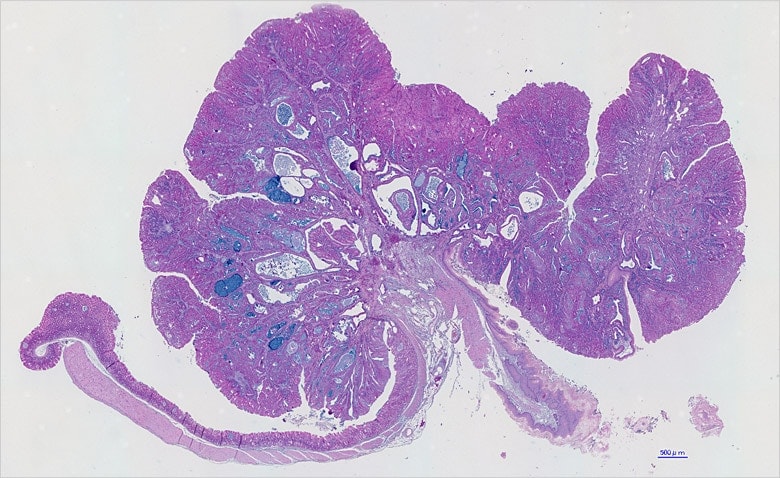
Wide-area image of mouse stomach obtained from image stitching on the BZ Series. There are absolutely no seams or unevenness. The organ size is approximately 18 × 12 mm.
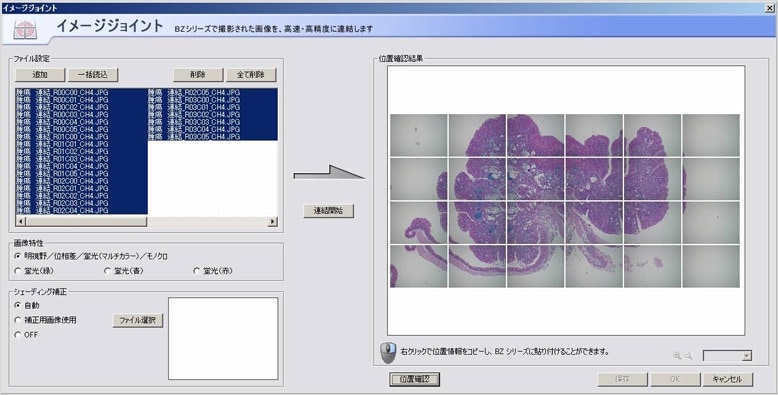
Operation screen of the BZ Series image stitching function. Multiple images can be joined together with simple operation.
We’re here to provide you with more details.
Reach out today!
07. Clear images obtained with haze reduction function
Dr. Ishimoto comments that the BZ Series enables the capturing of clear images with simple operations.
Co-researcher Dr. Takatsugu Ishimoto also frequently uses the BZ Series in the Saya Laboratory. Currently, he is engaged in research into the development of stomach cancer. Recently, the involvement of Helicobacter pylori has been identified as a cause of stomach cancer, but its mechanism in vivo has not yet been completely clarified. Through research using transgenic mice, Dr. Ishimoto is trying to discover, at a molecular level, the mechanism of how stomach cancer develops.
Dr. Ishimoto uses the BZ Series to observe entire mouse stomachs and sections of mouse stomachs.
“Conventionally, observation of tissue sections using a fluorescence microscope was not something you could do easily—it was far less accessible or approachable than it is now. First, if you wanted to observe something, you needed to prepare slides with specimens, and then carry those slides as you ran over to the darkroom in a different building. This was a major hassle.Regarding this issue, the BZ Series is very useful because it can be placed inside the lab and can be used any time we need it.”
Dr. Ishimoto says that he uses the BZ Series almost every day when there are many experiments to carry out.
“What is most appealing is the clear images. I find the haze reduction function, which eliminates fluorescence blurring, to be very handy. It can clearly show the target cell development and produces convincing images.”
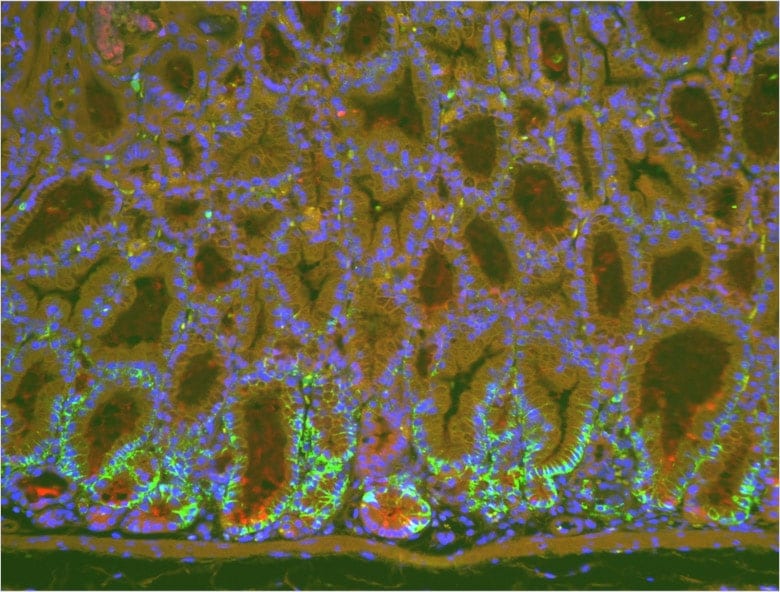
Fluorescent magnified image of stomach before using the haze reduction function. The green part is the gastric mucosa epithelium suffering from metaplasia as a result of chronic inflammation. The red part is the mucoid secretion from the epithelium.
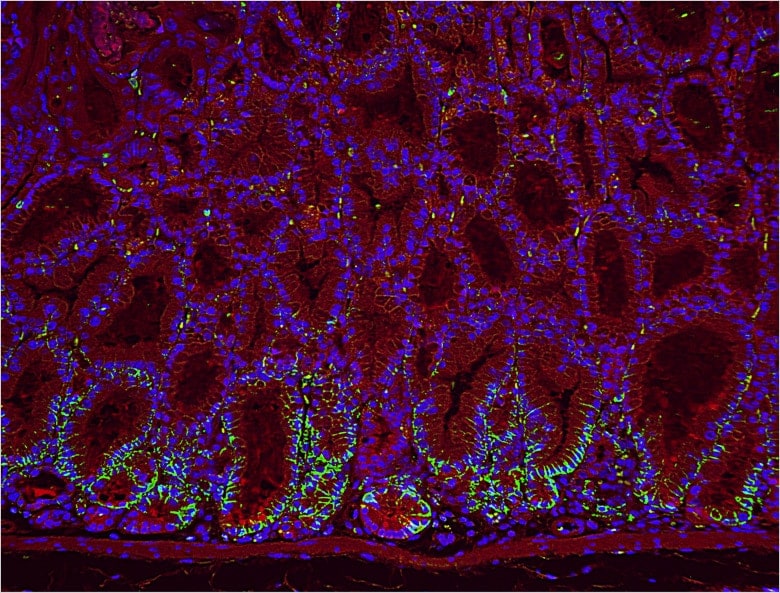
Image after processing the above image with the haze reduction function. Fluorescence blurring has disappeared, producing a clear image.
We’re here to provide you with more details.
Reach out today!
08. BZ Series used to capture all images for a paper
Dr. Ishimoto says that the BZ Series also contributes to the streamlining of research. “I use the cell count function to count target cells. It is very useful because it counts quickly and accurately. Previously, we used to hold a counting device to count each cell manually, but this took about half a day. Using the cell count function, the same counting can be performed in a matter of seconds.”
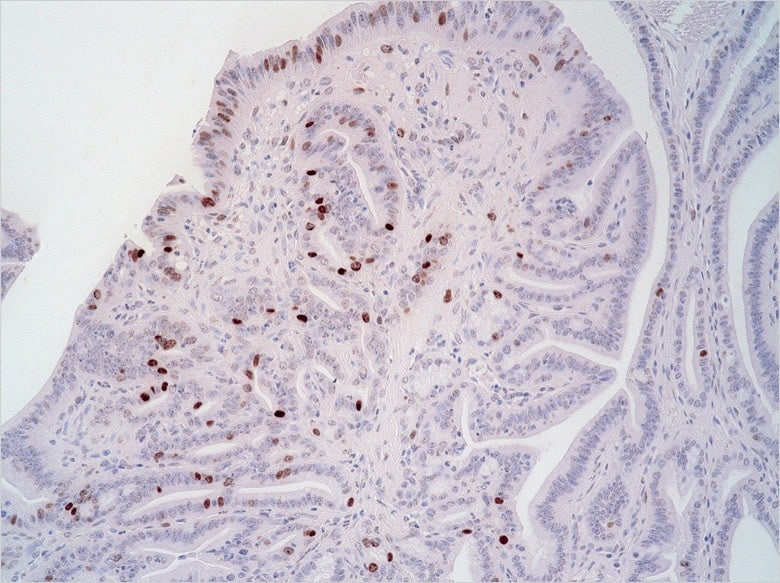
Cancer cells proliferating in stomach tissue. Original image before using the cell count function.
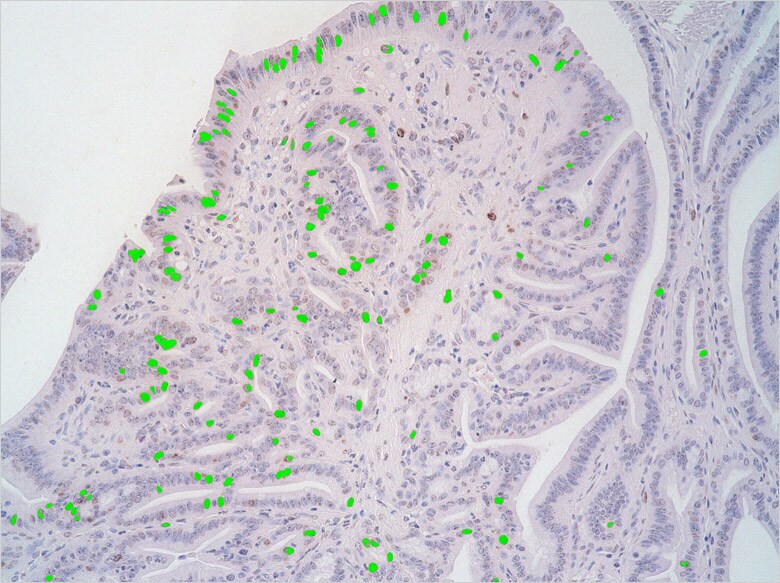
Image after using the cell count function. Cancer cells are marked in green, making it possible to perform automatic counting.
Dr. Ishimoto also mentions that the software is easy to operate, enabling anyone to use it intuitively.
The lab also has a confocal microscope, but it has rarely been used since the BZ Series was installed. Dr. Ishimoto explains, “As the confocal microscope is shared among laboratory members, we need to make a reservation first, which means that we cannot use it immediately at any time that we want.However, the BZ Series is close at hand and can be used at any time. Additionally, it is very convenient as we can complete all the tasks necessary for research—such as observation, image capturing, and cell counting—with just a single instrument,” highlighting some of the benefits of using the BZ Series.
Dr. Ishimoto is currently working on finishing up his paper for presentation at a conference. The images used for the presentation were all taken with the BZ Series.
“The mechanism of the development of stomach cancers and other gastroenterological cancers has yet to be fully understood. On the other hand, there is progress in the research on breast cancer and leukemia. Personally, I want to contribute to cancer treatment by clarifying the mechanism of the development of gastroenterological cancers.”
We’re here to provide you with more details.
Reach out today!
09. Possibility of substantial changes to cancer treatment

Dr. Saya talks about his hopes to “contribute to society by achieving drug discovery built on the accumulated findings from basic research.”
Dr. Saya’s cell-based research using iCSC has the potential to become the standard method of screening for cancer drug discovery. Aside from cancer, it is also considered a promising approach for genetic diseases and metabolic diseases.
Dr. Saya’s highest aspiration is to discover a treatment for brain tumors and other refractory cancers. He hopes to provide a foundation that enables doctors to provide the same drug therapies around the world. “My dream is to make brain tumors curable with oral medication,” says Dr. Saya.
The future progress in the cutting-edge research using iCSC will identify cancer development mechanisms and drastically change the concept of cancer treatment. Cancer, which is currently the number one cause of death, may someday cease to be a terminal illness.
(As of March 2009)
We’re here to provide you with more details.
Reach out today!
<General knowledge> Induced cancer stem cells (iCSC)
An induced cancer stem cell is a cancer stem cell artificially produced by applying the iPS cell production technique. It is possible to create induced cancer stem cells (iCSC) that generate a malignant tumor by genetically engineering the hematopoietic cells and bone marrow stromal cells of a mouse. iCSC will significantly contribute to drug discovery for cancer treatment. iCSC may also be useful in understanding the underlying mechanisms in cancer development, which is currently an unresolved question in the clinical application of iPS cells.