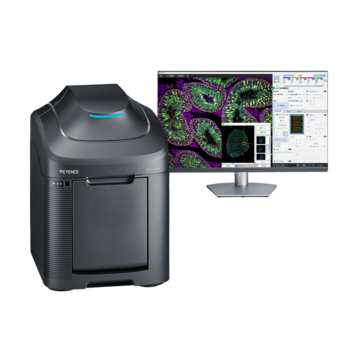
Fluorescence Microscopes
Developing Cell Sheets for Myocardial Regenerative Treatments

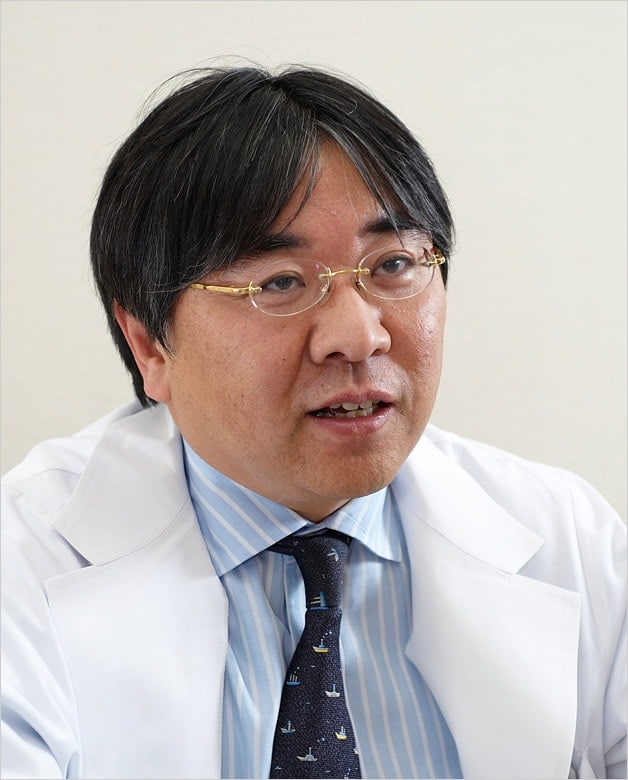
Dr. Yoshiki Sawa
Professor of Cardiovascular Surgery, Surgical Medicine, Osaka University Graduate School of Medicine
Center Director of Medical Center for Translational Research, Osaka University Hospital
Doctor of Medicine
Dr. Yoshiki Sawa was born in 1955. In 1980, he graduated from the Osaka University Faculty of Medicine and entered the First Department of Surgery at Osaka University. In 1989, as a Humboldt Foundation Fellowship student, became an exchange student studying under the cardiac surgery and cardiac physiology departments of the Max-Planck Institute in Germany. After his return to Japan, he became an Assistant to the First Department of Surgery at the Osaka University Faculty of Medicine, a senior member of the medical staff and lecturer. Then in 2002, he became Associate Professor of the Department of Organ Regulation Medicine (First Department of Surgery) at the Osaka University Faculty of Medicine. He was also appointed Assistant Director of the University Hospital’s Medical Center for Translational Research. In 2004, he was appointed Assistant Chief of Cardiovascular Surgery at the Osaka University Hospital. In 2006, Dr. Sawa was appointed both Professor of Cardiovascular and Respiratory Surgery, Osaka University Graduate School of Medicine, and Director of Osaka University Hospital Medical Center for Translational Research.
Get detailed information on our products by downloading our catalog.
View Catalog
The growing global interest in cell sheet treatment as a third treatment option for patients with critical cardiovascular disease
Dr. Yoshiki Sawa is the Head Professor of Cardiovascular Surgery, Surgical Medicine of the Osaka University Graduate School of Medicine. While standing at the forefront of clinical medicine, he continues to research the treatments of critical cardiovascular diseases with extreme fervor. In 2007, he was the first in the world to successfully treat a dilated cardiomyopathy patient by regenerating the function of the heart. This treatment was conducted by extracting muscle cells from the patient’s own leg, culturing the cells to create a cell sheet, and then transplanting this sheet onto the heart, resulting in the regeneration of its movement. In addition to conventional heart transplants and auxiliary artificial hearts, this new method is gaining interest around the world as a third treatment option to save patients with critical cardiovascular diseases.
We’re here to provide you with more details.
Reach out today!
01. Thorough investigations into cutting-edge medical treatments carry on the traditions of the former “First Surgery” Department
The department of Cardiovascular Surgery, Surgical Medicine (formerly called the “First Surgery” Department) of the Osaka University Graduate School of Medicine, carries the tradition of being the leading developers of surgical medicine in Japan. Beginning with Dr. Fritz Hertel, the department’s first professor; Dr. Yoshio Ozawa, the true founder of the program; and the second Professor, Dr. Yoshiaki Takeda, each Head Professor has continued the tradition of pioneering advanced surgical treatments. This department has a history of continually challenging and setting the trends of cardiovascular surgical treatments. As examples of this history, past members of this department include Dr. Hisao Manabe, the first person in Japan to successfully conduct open heart surgery using an artificial heart-lung apparatus more than half a century ago; Dr. Yasunaru Kawashima, the global authority on artificial organs and the surgical treatments of complex cardiac anomalies; and Dr. Hikaru Matsuda, whose efforts reopened the door to heart transplants.
Furthermore, this department boasts the highest success rate in the country for open-heart surgeries, regardless of the high rate of acceptance of critical cardiovascular patients. The department has also achieved the highest-ranking AAA rating of cardiovascular surgical treatment facilities according to the Nikkei (Japan Economic Newspaper).
Carrying on with this tradition, Dr. Yoshiki Sawa fulfills his role as Head Professor by breaking new ground in truly unexplored research territories. His goal is to find safe cardiac surgery practices and breakthroughs in the treatment methods of intractable cardiovascular diseases.
In terms of safe cardiac surgeries, Dr. Sawa refers to surgical procedures such as off-pump bypass surgeries that are minimally invasive and conducted without using an artificial heart-lung apparatus. He also refers to the treatment of aneurysms using stents (a network of metal tubes). Dr. Sawa’s approach to finding treatments is by “not always solving surgeries by simply using the scalpel, but rather through new technologies that are thought to be useful and that should be used in the best interest from the patient’s point of view.”
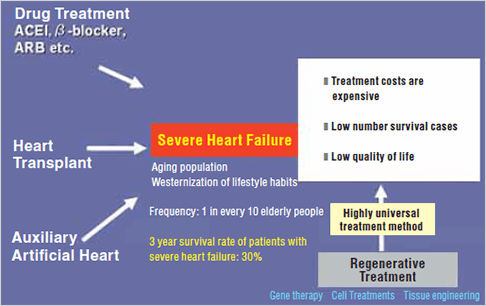
Treatment strategies against severe heart failure. The objective is to find a universal regenerative treatment method.
Dr. Sawa also states, in regards to the treatment of intractable cardiovascular diseases, “overcoming serious heart failure is our primary mission.” With this mission in mind, he is investigating the possible treatment methods from the standpoints of both heart transplants and auxiliary artificial hearts. Despite this, these types of surgical treatments do not necessarily recover the function of the cardiac muscle itself. To overcome this hurdle, Dr. Sawa is undertaking research into the regenerative treatment of the cardiac muscle.
We’re here to provide you with more details.
Reach out today!
02. The world’s first successful myocardial regeneration treatment using automyoblast cell sheets
The first attempt made by Dr. Sawa was a method in which the patient’s own automyoblast cells were implanted into his or her heart. Although there were definite treatment results with this method, Dr. Sawa acknowledged the importance of the administration method of myocardial cells to further increase the effectiveness of this treatment. For this purpose, Dr. Sawa teamed up with Dr. Mitsuo Okano, Professor at the Tokyo Women’s Medical University, and with their combined trial-and-error experiences over the course of 8 years, they developed a new treatment method. This new method used automyoblastic cell sheets to achieve myocardial regeneration.
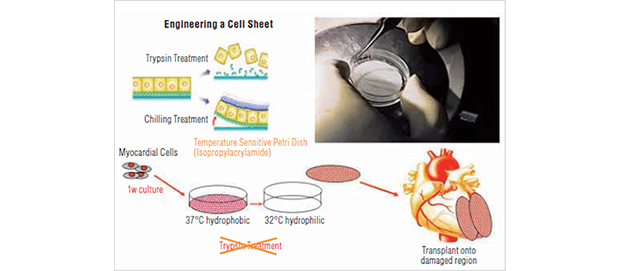
Development of myocardial regenerative treatment using a myocardial sheet. Cultured cells are transplanted onto the damaged region of the heart to achieve functional recovery.
In May of 2007, Dr. Sawa’s team was the first in the world to successfully implement this treatment method in dilated cardiomyopathy patients. First, muscle cells were extracted from the patient’s own leg and cultured. Then, these cells were placed in a sheet with a diameter of approximately 4 cm and a thickness of approximately 0.1 mm. This sheet was then transplanted onto the heart, and the successful regeneration of the heart muscle function was achieved. Prior to receiving this treatment, the patient had an auxiliary artificial heart in place and required a heart transplant to survive. 3 months after this treatment, however, the contraction rate of the heart had improved, and the volume of blood being transported around the body recovered to the point that the auxiliary artificial heart could be removed. By December of that year, the patient’s condition had improved to the extent that the patient could be discharged from the hospital.
The effective cell engraftment associated with this treatment has lead to high regard for this method, thereby resulting in the treatment being referred to as the third treatment option together with heart transplants and auxiliary artificial hearts, giving hope to patients who suffer severe heart failure.
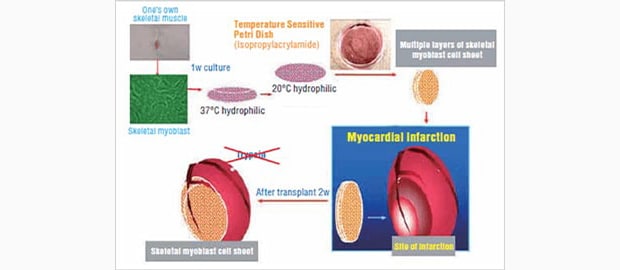
Treatment using a skeletal myoblast cell sheet. This technology is currently being patented.
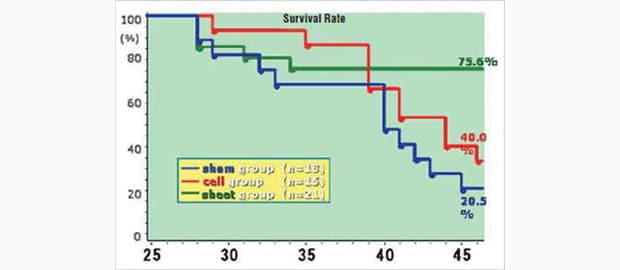
Myocardial regeneration according to the skeletal myoblast cells in DCM hamsters. The survival rate of hamsters that have been treated with sheet cells (green line on the graph) is considerably higher than the other hamsters.
* Myoblast cell: these cells make up the muscle fibers that are the structural elements of muscle tissue. Single nucleus myoblast cells multiply, and then these cells are assimilated into myotube cells, finally becoming the muscle fiber.
We’re here to provide you with more details.
Reach out today!
03. The Medical Center for Translational Research: Establishing regenerative medical treatments

The approach of the Medical Center for Translational Research of the Osaka University Hospital. As stated above, in addition to propelling the research directly toward the future of medical treatment, the center acknowledges the importance of translational research.
Before achieving this feat, Dr. Sawa also undertook research into regenerative treatments, working towards the establishment of a comprehensive system. In 2002, with the aim of translational research, he became the Assistant Director of the Medical Center for Translational Research, placed within the Osaka University Hospital. Through this management position, he was able to collaborate with the facilities and personnel required for regenerative treatment (in 2006 he became the Center Director).
In the culturing of the automyoblast cells that are essential to regenerative treatments, Dr. Sawa established the CPC (Cell Processing Center = cell culture manufacturing preparation facility) conforming to GMP (Good Manufacturing Practice). Furthermore, through the development and positioning of necessary staff, Dr. Sawa has used every possible means to build a comprehensive treatment system.
Regarding this development, Dr. Sawa was quoted as saying the following.
“As there has been no one before that has attempted this approach, we began by groping our way around blindly in the dark. Through the assistance and support of both the government and the pharmaceutical industry, we have finally been able to strengthen this system.
This center is a clinical research center that is a go-between that supports the development of new treatment methods aimed for the future. As this center is a facility of the University, research is not limited to fundamental research, but continues the investigation into steps to save critical patients with no other alternatives from a clinical standpoint. The ultimate objective of this center is to be a cell culturing factory that acts as a backup for regenerative treatments.”
We’re here to provide you with more details.
Reach out today!
04. A desire to save just one more patient from severe heart failure
Dr. Sawa continually pursues medical treatments aimed toward a new era. He began his medical journey because of the influence of his grandfather, who was a medical practitioner. His resolve to become a medical doctor solidified when his cousin was killed in a road accident during his teenage years.
In the years that followed, Dr. Sawa exercised his ability as an open-heart surgeon and saved many patients. However, he also had to endure the many patients he lost without being able to help in the many years during which heart transplants were not recognized in Japan. Even now, when transplants from brain-dead donors are accepted, the number of transplant surgeries that can be performed is limited due to a shortage of donors. The strong fundamental need to fulfill his obligations as a doctor lies behind his drive to make regenerative treatments a reality.
Dr. Sawa does not see the cell sheet, a world first, as the final goal in regenerative treatments. To achieve treatments with further effectiveness, he is also considering the use of iPS cells. The creation of myocardial cells based on iPS cells followed by the creation of a sheet from these cells leads to the continued promise of a treatment method.
* iPS cell: This term stands for induced pluripotent stem cell. These are pluripotent stem cells that are created from somatic cells.Theoretically, any cell composition within the body can be created from iPS cells.
We’re here to provide you with more details.
Reach out today!
05. Increasing efficiency of experiments in order to transfer research results quickly to patients
Dr. Sawa is also a clinician in charge of outpatients. While sincerely facing critical patients, he feels strongly the need for regenerative treatments.
Dr. Sawa continues to vigorously progress his research with the aim of establishing the regenerative treatment of heart function. To save even one more critical patient with no other alternative, he is devoting himself to the speedy development of research treatments by increasing efficiency and decreasing the labor involved in his research. Of particular importance is the recruitment and training of the members of his research team.
According to Dr. Sawa, “it is important to, while fostering the young researchers, place the right people in the right positions and therefore heighten the motivation of each individual. By doing this, one plus one can equal three or more, and a research system with organizational strength can be created.” In addition to this, he is also taking into consideration the investment of facilities and equipment that may increase research efficiency.
He clearly states, “The key lies in reducing the amount of wasted time and effort during research activities. Particularly from the standpoint of competition on a global scale, speed is of the essence. Furthermore, I am fully aware that the faster we gain research results, the more beneficial to the patient.”
On the other hand, to break through to this previously unknown treatment method, Dr. Sawa points out “it is important to clarify the relationship between the benefits and risks involved in the introduction.” Speed but with poor results is unforgivable. Only when the relevance and safety of the treatment can be strictly proven during preclinical tests can the transition to human clinical trials be made possible. Dr. Sawa emphasizes the importance of “providing strict and objective evidence in the animal testing phase.”
Dr. Sawa, who as a young man acquired his doctorate by researching using an electron microscope, attaches great importance particularly in gathering evidence from a histological standpoint. “The conclusive factor that objectively proves whether, for example, cells have propagated, can depend on whether a definitive photograph has been taken. Of course, the numerical data of the experiment is also important, however, it is not an exaggeration to state that a single photograph can change the value of a thesis. For this reason alone, in the coming years it will become essential to use a microscope that links with the efficiency of observations and has superior abilities.” says Dr. Sawa.
We’re here to provide you with more details.
Reach out today!
06. Easy observation of a rat heart, from the entire heart down to the cellular level

Mr. Kenji Miki, operating the “BZ Series” in the laboratory
The man researching the regenerative treatment of myocardial functions on the basis of the research principles laid out by Dr. Sawa is Mr. Kenji Miki, who is currently enrolled in the Masters Course. He is undertaking research related to the formation process of everything from myoblast cells to myotube cells and over the past year has been observing the hearts of rats each and every day.
The device he is using to assist in this research is the KEYENCE BZ Series fluorescence microscope. The function of particular use is the multi-dimension time-lapse function, which can capture the images of cell changes over time. The myoblast cells transplanted onto the rat heart can be monitored to observe whether myocardial regeneration has occurred over time by capturing and saving these images. Furthermore, the Z-stack image capture, a function that can capture images along the vertical axis and generate a fully focused image, is also being used.
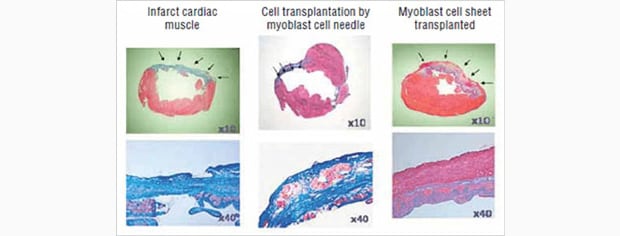
From the left, comparative images of: heart under myocardial infarction; heart with myoblast cells inserted; heart with sheet cells transplanted. The heart with the sheet transplant on the right is showing good cell engraftment.
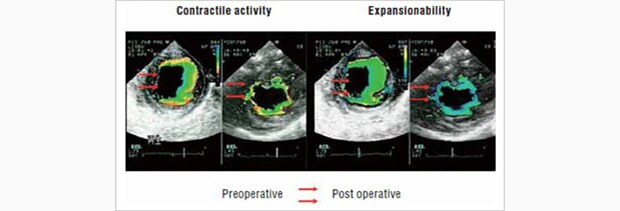
Transplant results of a myoblast cell sheet using a pig infarction model. The recovered function of the heart can be seen.
The main research Mr. Miki is undertaking is an investigation into the most efficient method of conducting myocardial regenerative treatments using cell sheets, a treatment method that was successfully utilized by Professor Sawa. For this research, Mr. Miki has developed a cell sheet based on a new network design, improving on the conventional round sheet. Through layering, he has created an environment where cells can easily be incorporated, and through this method, he hopes to improve the regenerative effects. In this type of research, Mr. Miki expresses the advantages of using the BZ Series by saying,
“to be able to observe the changes in the myoblast cells that are spread over a wide range over time is indispensable. However, the greatest advantage is being able to observe multiple points (up to 30) with time-lapse images. On top of this, the images are clearer than anything I’ve worked with before. There are many occasions where I use the observation images of different microscopes, but the color-definition of the BZ Series is clearly a cut above the rest.”
The diameter of a rat’s heart is approximately 1 cm. To gain an understanding of the regenerative condition of cells, the heart must be observed through images of the entire heart at an extremely weak angle. Then, the ability to perform magnified observation of the percentage of myoblast cells existing within the cell sheet is vital. By using the BZ Series, the two stage macro and micro observations are supported and conducted with ease.
“When looking at published research papers up until now, there were many localized images that showed only the heart’s infarct section and its boundaries. Being able to provide images of the entire heart enables me to strive for theses that are strongly persuasive.”
According to Mr. Miki, one of the great appeals of the device is how easily it can be used from an installation on a desk, not even requiring a darkroom for imaging. The device can be placed in a corner of the laboratory and can be used with minimal training. Furthermore, the optional temperature and CO2 regulation chamber can be used to easily conduct raw cell time-lapse observation over long periods of time.
We’re here to provide you with more details.
Reach out today!
07. Image processing that at one time took an entire day can now be completed in an hour
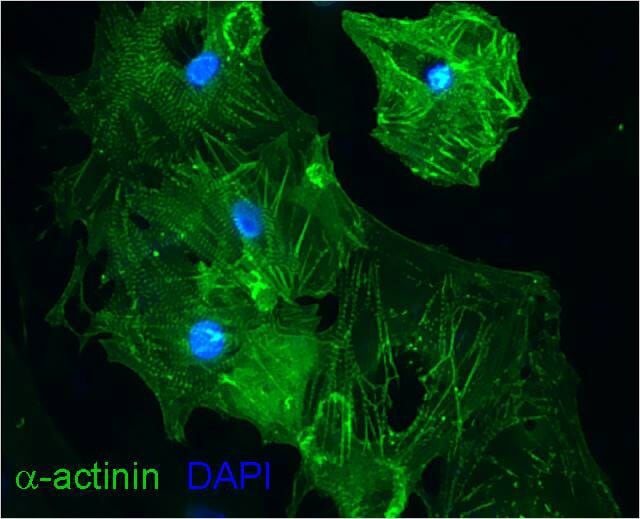
Differentiation-induced myocardial cells from iPS cells. The cytoskeleton is clearly stained.
(Image captured by the KEYENCE BZ Series)
In addition to the ease of observation, the BZ Series also exhibits a labor-saving benefit after images are captured. Up until now, Mr. Miki would first upload images taken to the PC, and then use image processing software to superimpose images with differing fluorescent colors. He would choose from a large volume of images the ones that were most focused, and then spend countless hours superimposing red, blue, and green fluorescent colored images. Despite the long hours, there was also no guarantee that the images were always clear.
In such a case, by using the best focus function of the BZ Series, the images with the best focus from the large volume captured on the Z-stack are automatically extracted. Furthermore, these extracted images can also be edited in chronological order. Mr. Miki admits “there were even times where an entire day was wasted simply on compiling images.” But after using the BZ Series, Mr. Miki explains, “processing can be completed in an hour, reducing the man-hours to 1/10th of the time that was previously needed.”
By substantially increasing the efficiency of observation, image capturing, and post-processing, Mr. Miki states that “we are now able to pursue research results with even higher accuracy.” This ability can be attributed to the wide range of experiments that can incorporate this device, making the work much easier. Observations that were previously abandoned, as they were too time-consuming, are now possible. Furthermore, the number of images captured, to prove research results, has been substantially increased. It can even be said that Mr. Miki—through the use of the BZ Series—is achieving the “objective proof” that Professor Sawa is seeking. Mr. Miki truly appreciates the image quality, as all images used in experiment records and for conference presentations have been captured using the BZ Series.
Today, Mr. Miki is undertaking a new approach, researching the methods of producing large amounts of myocardial cells using iPS cells. Currently, throughout the world there are many cases of research being undertaken around differentiation induction of the heart muscle. However, even if differentiation induction takes place, this is limited to only a few tens of thousands of cells. Mr. Miki is pursuing the establishment of technology that secures a minimum of a few million cells being produced, which is essential in the creation of a regeneration treatment sheet. By obtaining a large quantity of myocardial cells, the regenerative treatment using cell sheets will be a large step closer to becoming a reality.
We’re here to provide you with more details.
Reach out today!
08. Seeking future medical treatments through the Advanced Blood Vessel Treatment Course
Dr. Sawa, in addition to exerting every effort in pursuing the treatments of patients as a clinician, is attempting to establish a regenerative treatment system as the Center Director of the Medical Center for Translational Research. The objective is to literally indicate the direction of future medicine. That is, providing highly safe medical treatments and the development of treatment methods for cardiovascular diseases where currently no treatment methods exist.
“To achieve this we must go beyond the boundaries of current surgical and internal medicines by taking the better parts of each and integrating them. In a manner of speaking, on the basis of the concept of a ‘Surgical Circulatory System Course,’ we are embodying a new kind of medicine. The regenerative treatment of heart function that we are currently undertaking is an example of this. On the basis of definitive fundamental research, we wish for future medicine to quickly reach human clinical trials.”
In April of 2007, Dr. Sawa created a contributory course called the “Advanced Blood Vessel Treatment Course.”The idea is to, through this course, push beyond the barriers of surgical and internal medicine treatments. We wish to treat diseases by supporting the patient from both sides, using surgical means on one side and internal medicine on the other. This is the ideal treatment system that Dr. Sawa wishes to achieve. Dr. Sawa is not satisfied simply with standing at the forefront of medical research, but rather, you can feel his strong will and desire to greatly change the entire face of medical treatment.
(As of December 2008)
We’re here to provide you with more details.
Reach out today!
<General knowledge> Gene therapy for cardiomyopathy
Conventionally, the medical norm for patients with myocardial infarctions due to diseases like ischemic cardiac disease was that once myocardial cells became necrotic, there was no chance of recovery. In recent years, research into the regeneration of function through the transplanting of myocardial cells to the heart muscle is progressing.